To be healed does not mean to be cured. Cure restores a former state of being, an expected state, a comfortable state. Medical treatment and prayers for miracles of cure are powerful and sometimes effective. Healing, however, encompasses a much greater and deeper change in someone’s life. Cure may be part of this, but is not a necessary part. Healing opens up a new life, a new way of understanding oneself, a new way of loving others. Healing may not be physical, it may be emotional, psychological or relational. Culturally, there has been an increasing expectation of cure, and the medical accomplishments of the last century are truly incredible. At the same time, however, these expectations can make healing more difficult, especially at the end of life where people may become angry that they could not be cured, and fearful of dying. Thankfully, palliative care, with the emphasis of healing rather than cure, is gaining increasing support and acknowledgment.
I am not an expert, but I have had the privilege of working in a hospice. This essay is therefore a tribute to the enormous dignity of the patients, relatives and staff at the place where I worked. I hope to give a brief introduction to palliative care, and why we need to emphasize the dignity of this experience. In the U.K., the debate about dignity has to be done in secular terms in the public forum, since references to God are frequently dismissed as irrelevant. However, I will also look to Our Lord’s experience of death, and the wisdom of the Church for what guidance may be found there. Finally, I wish to emphasize the role of every member of the Church, since death is a universal phenomenon, and we all share in the responsibility of upholding the dignity of dying people in our community.
Dignity: To choose to live until death, or to die before the natural end?
Palliative care often begins with the acceptance that a particular illness is not going to be cured. Recent times have seen palliative care play a role earlier on in a disease process, not just in the final few weeks or days of life. Medical care does not cease, nor does treatment necessarily; however, the focus shifts from aiming for cure and prolonging life to aiming for comfort. Palliative care is often described as a holistic specialty, because in addition to the medical intervention that is dedicated to symptom control, there is recognition that psychological, emotional, spiritual and social circumstances play an equally important part in someone’s wellbeing. The impact of ‘non-physical’ circumstances or states on symptoms such as pain and breathlessness should not be underestimated.
Since the beginning of the modern hospice movement, palliative care has become an increasingly important part of healthcare, helping people live until the end. Dame Cecily Saunders, who founded St. Christopher’s Hospice in London in 1967, said this:
You matter because you are you, and you matter to the end of your life. We will do all we can not only to help you die peacefully, but also to live until you die.
This has inspired a global change in the attention given by the medical profession to people at the end of their lives. More recently, however, there has been a rise of an alternative view: the desire to help people to die before the natural end. This is often proposed in the name of dignity and the relief of suffering. Both sides of the debate claim dignity as a goal. How do we reconcile these differing understandings?
The Oxford English Dictionary defines dignity as “the quality of being worthy or honorable; worthiness, worth, nobleness, excellence.” The clash of opinion over dignity seems to be partly attributable to whether the term ‘dignity’ should be applied to the person, or to the circumstances of the person’s death. Is it the individual who is unchangeably dignified and worthy of a particular respect and honor until the end of life, or is dignity something that can be lost towards the end of life, alongside the loss of continence or muscle strength?
One of main pro-assisted suicide campaign groups in the U.K. claims dignity in its title: Dignity in Dying. Dignity in Dying believes that:
Everyone has the right to a dignified death. This means:
- Choice over where we die, who is present and our treatment options.
- Access to expert information on our options, good quality end-of-life care, and support for loved ones and carers.
- Control over how we die, our symptoms and pain relief, and planning our own death.
This use of the word “dignity” is as an attribute of the death, something that is contingent on circumstances, rather than being inherent to a person. It is deemed to be undignified to lose one’s capabilities, to be dependent on the care of others, to be in pain and suffering.
The alternative view, as demonstrated by David Jeffrey, a palliative care physician, is as follows:
Dignity is intrinsic to humanity and not dependent on particular characteristics, such as intelligence or disability, but is present in every living person. It is something which cannot be lost and should be respected by others even if an individual no longer values it for him.[1]
He points to research that shows that patients do not consider control over the timing of their death to be a feature of dignity.
Admittedly, changing the definition of dignity may not change the pro-assisted suicide campaign, which would likely continue to fight for control over the timing of death. People who propose euthanasia or assisted suicide believe they are doing right by campaigning for the alleviation of suffering and for individual choice. Showing that someone is not diminished as a person and cannot lose dignity because of the suffering he or she undergoes, however, may be helpful in our reconciliation with death and the unpredictability of the dying process.
Dependence is Dignified
A crucial element of discussions about dignity towards the end of life seems to be the loss of dependence and the loss of control. Why is becoming dependent so challenging? There is a tension in human life between our identity as individuals, who like to think we have independent thought and enjoy a sense of self-determination, and the basic fact that humanity only continues to exist through society, upon which each individual depends for a wide range of things from basic existence to whether there is a carton of milk in the fridge. Community and humanity only exist because of interdependence.
This tension has become starker in recent times with the rise of the individualistic culture. In medical ethics, autonomy has frequently become the prime consideration in decision-making, giving patients more control over their treatment. This has brought many benefits, and treatment is better when a patient is involved and in agreement. However, sometimes autonomy unrealistically eclipses all other considerations, since ultimately a stable society cannot function well without wider considerations.
So what is it about being dependent at the end of life that can make some people feel less human, less valuable? At the beginning of life, we are vulnerable and completely dependent on our mothers. Yet even here there is a tension, for we are within another’s body (what could be more dependent?), and yet still an individual. Once we are born, whilst there is a greater degree of physical detachment, a healthy baby still needs constant attention. As a child grows, the type and degree of dependence changes. No one would credibly argue that it is undignified for a baby to have its nappy changed. Indeed the reverse is true: to leave someone who is incapable of changing his nappy is to leave him in an undignified state. So why is it undignified for an adult who is incapable of getting up from a bed to use a toilet to have a soiled pad changed? Is it because there is a need for such an act itself, or is it perhaps the attitude towards such a need, both from the individuals who have the need and those who attend to them?
Perhaps it is the awareness of incapability, since human beings strive for perfection and development. Losing a capability, if the ideal of perfection is based on one’s usefulness, feels like a step away from our goal. We are more aware of incapability as a negative thing when we compare ourselves to others, and when others compare us to themselves. And so our feeling of dignity is not so much something that arises from an individual as something that arises from society and the attitude of others towards those who are dependent on them. Dignity in this light is an unstable concept, which varies with time and people. This is described by Jonathan Herring as follows,
A person’s sense of dignity in part depends on how they are treated by society and those they relate to. If a person at the end of their life is feeling undignified this may say as much about our society’s attitude towards the elderly and dying as it does about an individual’s own values.[2]
In a comment in the British Journal of General Practice, Peter Aird explains that, “we all need to be happier to help.” He is saddened by celebrity support for assisted suicide, concerned by the attitude that being a carer ruins one’s life. However, his experience is that there is satisfaction and joy to be had in caring. He reminds us that
humans are meant to live in a community, supporting one another. And if we all want to be needed, then some of us are going to be those who have needs.[3]
Recently, whilst working in the emergency department, I have seen two older ladies who have attempted suicide, both of whom had written lengthy letters to their families saying that they “did not wish to be a burden.” This made me reflect on social influences on illness. The biopsychosocial model of health and illness is commonly used to describe the factors influencing psychiatric illness. Whilst depression certainly has biological and psychological factors, we must not underestimate the potential influences of societal attitudes. If society, and celebrities in particular, continue to promulgate the message that one should not be a burden, and are better off dead than suffering, there is surely no doubt that this could pressure a depressed older person into considering suicide. Of course, the biological and psychological factors in depression mean that suicide cannot necessarily be prevented by the care and attention of others. However, social factors such as loneliness, feeling abandoned by family, or even the sense that family have more important things to do with their busy lives can have an enormous influence.
Worthy Suffering?
The other aspect of the dignified death is the question over the worth of suffering. John Wyatt has this to say:
In a modern secular worldview, suffering seems to have no ultimate meaning. It is pointless and destructive, the ultimate threat to individual human autonomy and self-direction. Therefore, suffering is an evil to be eliminated by whatever means are to hand. It is natural that the elimination of suffering has become, for many, the prime goal of medicine, as well as the fundamental motive behind all utilitarian philosophy. It is an easy step to accept that, in the name of eliminating the suffering, we are forced to eliminate the sufferer.[4]
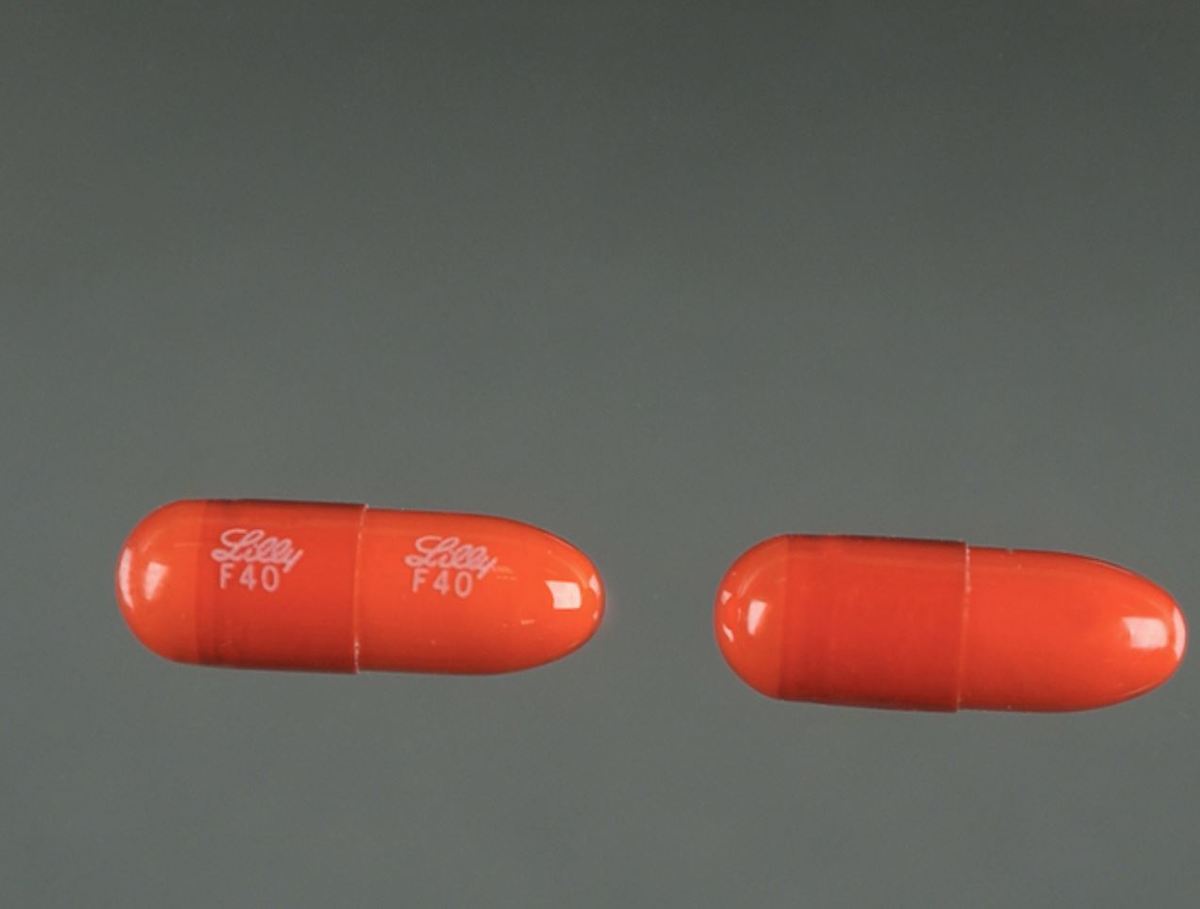
Pain and suffering are cited as reasons to bring about an early death. In the hospice, many patients had pain, most of which could be treated with standard medication. But even those who had pain that was difficult to treat went through the slow process of finding effective treatment. This did not always result in zero pain, but the improvement gave respite and stopped pain from being the overwhelming experience of the final days or weeks.
It is crucial to remember that often the most difficult pain to treat is not physical pain; the “problem pain is spiritual pain, emotional pain, relational pain.”[5] This should be an encouragement to all: you can play an important part in alleviating pain; you do not need my medical degree. You can make peace, you can encourage, you can visit the dying, and your contribution will remind someone of his dignity, his worth.
Careful to Care
This may be stating the obvious, but calling something ‘palliative care’ does not grant automatic immunity to any violation of dignity. Individual situations can be very complex, but there are some practices that come under the umbrella of palliative care, which may not always maximize the dignity of each person. For example, Jeffrey discusses the use of sedation at the end of life. Palliative sedation in the U.K. means the careful titration of sedatives in order to relieve distress. The process is monitored by clinicians and sedation is reduced if symptoms subside. However, terminal sedation is on the rise in the Netherlands. There, it can be used with the intention of hastening death, but does not carry the same reporting obligations of euthanasia and physician assisted suicide.[6] Intention, both of the caregivers and the individual being cared for, plays a crucial role in some aspects of palliative care, and can alter the morality of a practice. We must keep the dignity of every moment of a person’s life at the forefront of end-of-life care.
Walking with Jesus
As I have explained, palliative care does not strive for miracles of cure, but accepts the inevitability of death. It could be said that Jesus is not a great example for us in the field of palliative care: being God, he could and did cure people who were dying, and raised people from the dead. However, when it came to his own Death, Jesus did not try to escape from the inevitable, and accepted every suffering along the way. Whilst Jesus’ Death was more violent, unnatural, and brief than the sufferings of someone who has cancer or heart failure, it nevertheless can be our model.
I invite you to reflect on how the Passion of Christ might guide your own experience. This might be as a dying person who takes up his cross (Mt 16:24), uses this time for reconciliation (Lk 23:42), and considers how family members are going to cope after he has passed away (Jn 19:26). You might experience the feeling of desertion and loneliness (Mt 27:46) and yet be able to say, in the end, “Father, into your hands I commend my spirit” (Lk 23:46). As a carer, you may find yourself unexpectedly and perhaps undesirably in the caring role (Mt 27:32). You may be watching the suffering of someone you love, and be unable to help (Mt 27:55). You may be able to provide some physical comfort, or you may only be able to watch at the foot of the cross (Jn 19:25). As well as direct scriptural references, the tradition of the Stations of the Cross gives us the opportunity to meditate on death and dying.
None of us wishes to die in a painful or unpleasant way, and we are right to seek to alleviate suffering where possible. Jesus refuses the gall and vinegar given to him on the Cross (Mt 27:34), which could be viewed as an invitation to endure the sufferings that are present and not seek to alleviate them. Pope St. John Paul II reminds us, however, that
while praise may be due to the person who voluntarily accepts suffering by forgoing treatment with painkillers in order to remain fully lucid and, if a believer, to share consciously in the Lord’s Passion, such “heroic” behavior cannot be considered the duty of everyone. (Evangelium Vitae, §65)
We do not have to prove our dignity and worth before the Lord by suffering as he did. However, we would be mistaken to think that suffering is necessarily undignified. Mathewes-Green says this:
We want our deaths to be free from pain, mess, embarrassment. But there is a long Christian tradition of "holy death," that is, of allowing even a hard death to be a witness to God’s grace. We’re nowhere invited to ring down the curtain early to preserve our pride. How dignified did Jesus look on the way to the Cross? Spattered with blood and spit, despised and rejected, he carried his own instrument of torture up a hill. Was this a death with dignity? Ironically, it was. The Latin root for dignity is dignus, which means worthy. The most worthy death in history was shorn of all dignity. Yet it was the death that transformed death, changing it from a wall to a door.[7]
The Church and Palliative Care
Beyond the Death of Jesus, what guidance does the Church offer? The Catechism of the Catholic Church says that “palliative care is a special form of disinterested charity. As such it should be encouraged” (§2279).
Palliative care is the name given to the care of the dying by the medical profession. Catholic healthcare professionals perhaps will see palliative care as a particular vocation, which the Church commends highly. But our understanding of palliative care should not be limited to official pathways and roles. In 2015, the Pontifical Academy for Life held their General Assembly with the theme of “Assisting the Elderly and Palliative Care.” In his address, Pope Francis recalled that:
The elderly, first of all, need the care of family members—whose affection cannot be replaced by more efficient structures or more competent and charitable healthcare workers. When this is not sufficient, or in the case of advanced or terminal illness, the elderly can be benefitted by truly human assistance, and receive adequate responses to their needs thanks to palliative care offered in such a way that it supplements and supports the care provided by family members.
Whilst the formal structures of palliative care are important, the family bears the first responsibility for their elderly relatives. This may be difficult and even life-changing for those of us with already busy lives and responsibilities, but our response to the needs of our own relatives have a great bearing on their wellbeing and sense of their own dignity.
Apart from the material and social needs of family members, we also have a responsibility to ensure that they receive the spiritual support they need. The Catechism instructs us that
the dying should be given attention and care to help them live their last moments in dignity and peace. They will be helped by the prayer of their relatives, who must see to it that the sick receive at the proper time the sacraments that prepare them to meet the living God. (§2299)
Some people may need help with attending Mass, or may be unable to attend, in which case we can help by arranging for them to receive the Eucharist at home. We must pray for those who are sick, and should help them to receive the Sacrament of the Sick in a timely fashion. Whilst it can be difficult to discuss death, a person approaching the end of his or her life may be reassured by talking about funeral arrangements and by knowing that someone will pray for their soul as they journey through purgatory and into the eternal life of heaven.
Beyond our immediate family, there are those members of our Church family to whom we also have a responsibility. Whilst we may not be able to fulfill the material needs of dying people in our parishes, there are many things that the Church guides us to do for their spiritual good. We may pray for those who are sick and housebound; we may visit them. We may attend the funerals of those in our parish, even if we only knew them by sight.
Apart from what we can do for others, there is a great emphasis in the Church on preparing for our own deaths, although perhaps the importance of this has been muted somewhat in a culture where healthcare is so good that we do not expect to die until old age. In the encyclical Evangelium Vitae, Pope St. John Paul II says:
as they approach death people ought to be able to satisfy their moral and family duties, and above all they ought to be able to prepare in a fully conscious way for their definitive meeting with God. (EV §65)
He reminds us that, as dying people, we ourselves have ongoing responsibilities. When we are cared for, we do not simply become passive recipients of other people’s attention. We still have a role to play, duties to fulfill, and a task to complete: that of preparing ourselves to meet the living God. It seems to me that this sense of purpose itself can be a great help in retaining our sense of dignity as well as the example we can show to others. The way that we die can have an enormous impact on other people, either in a positive or a negative way. The phenomenon of suicide contagion is well documented, and there are concerns that this extends into the effect of media coverage of assisted suicide. Alternatively, the media can have a preventive influence, by demonstrating how people have coped with and overcome suicidal feelings. We should remember the gifts that dying people offer to us, and the gifts that we will be able to offer as dying people.
Reaching Out
The way that we ourselves die may be a great witness to the world, and our approach to death must surely be a source of evangelization. To be able to offer the hope of ongoing eternal life, when the alternative is nothing, is a great opportunity. There are many things we can do for our fellow Catholics: continuing to preach the Good News to them, whether that be in words or deeds as an encouragement towards the end of earthly life. But what about palliative care in a multi-faith and secular environment? How can we give hope to those who do not know or accept Christ?
The end of life is an extremely vulnerable phase, emotionally and spiritually as well as physically. We should always remember that we do not evangelize in order to make other people ‘part of our club,’ to justify ourselves. We should never offer our service to the sick on the condition that people have to participate in prayer or listen to preaching. Deathbed conversions should not be our primary goal. We offer our care in order that people understand their own dignity, to make it easier for them to understand the worth of their lives at every moment. Through this, they may inquire about the reason for the hope that we have, and then we can have our answer ready (1 Pet 3:15–16). However, amongst the people I met at the hospice, few had faith or religion as a primary concern. Most were concerned about family, and support for families (cf. Jn 19:26); reconciliation of estranged relatives can also be a great source of comfort. We cannot know what is happening in someone’s heart, especially not in the final days or hours when someone can no longer communicate, but we must remember our merciful God, who will honor those equally who turn to him at the very last hour (Mt 20:1–16).
Conclusion
The human capabilities in medicine to heal and cure are the primary place that we turn to when we are unwell. However, when human ability to cure is outdone, there is a great task in our provision of care for others. Palliative care has been transformed in the last century in terms of the medical and other holistic care that is given to dying people. However, hospices are nevertheless formalized care, and are still places of professional-patient relationships. Those who work in a hospice environment perhaps spend more time with the dying, but the responsibility for the care of the dying does not lie only with professionals, but with each one of us. The boundaries of palliative care are, in fact, difficult to define since our personal relationships with others can have a huge impact on their experience of death and dying. In a fragmented society where families may be separated by breakdown of relationships, or physical distance, or even the busyness of everyday life there can be great pain and loneliness for those at the end of their lives. However, this means that there is a great opportunity for everyone to prepare for death and for the death of others by making peace with relatives and friends and by making time for those closest to us and those for whom we have responsibility or towards whom we have a duty. Palliative care extends to the whole of society, from the scientist developing pain-relieving medications to the doctor or nurse prescribing or administering medications, but perhaps most importantly to each and every one of us in remembering and upholding the dignity of each human life until natural death. Holy Mary Mother of God, pray for us now and at the hour of our death. Amen.
[1] David Jeffrey, Against Physician Assisted Suicide: A palliative care perspective (Oxford: Radcliffe Publishing, 2008), 23.
[2] Jonathan Herring, Medical Law and Ethics, 4th ed. (Oxford: Oxford UP, 2012), 521.
[3] Peter Aird, “Assisted Dying: We all need to be happier to help,” British Journal of General Practice 65, no. 637 (2015), 415.
[4] John Wyatt, Matters of Life and Death: Human dilemmas in the light of the Christian faith (Nottingham: Inter-Varsity Press, 2009), 219.
[5] Wyatt, Matters of Life and Death, 230.
[6] Jeffrey, Against Physician Assisted Suicide, 70.
[7] Frederica Mathewes-Green, “Dignity, always dignity” via World, February 18, 1995.